








Retired professional wrestler,
Entrepreneur, TV personality

Retired professional wrestler,
Entrepreneur, TV personality

The original “Wolf Of WallStreet”, entrepreneur, speaker,best-selling author.
There’s been a gigantic shift in the world’s economy…
While some people simply traded in their current job for a new one… Others started weird “side hustles”…
Like selling used lingerie, raising & selling baby goats and flipping couches.
Watch as Rudy Mawer scours the U.S. to uncover unique, weird and even stupid side hustle ideas which are generating a boatload of cash…
Not everyone will make the cut! These entrepreneurs will be put through the wringer first. Will it turn out to be just a “stupid side hustle” or a money-minting cash cow? Watch to find out!



Tune in to hear Rudy interview some of the sharpest minds in business sales, marketing and sports to give you the no-holds-barred truth about what it takes to take your life to the next level.
No wonder listening to Living The Red Life is quickly becoming a daily routine for thousands of ambitious entrepreneurs like you.

Rudy is one of the most famous business influencers and celebrity marketer in the world with his famous red brand, with over 1 million followers, 200 + stages as a Keynote speaker, TV shows and news interviews.
Rudy has successful TV shows on major streaming platforms and a top 10 entrepreneur podcast “Living The Red Life”. After 10+ years growing brands online, Rudy now works with famous Billion $ brands and major A-list celebrities to advise, consult and build out their social media strategy, their overall online business, and help with branding and vitality.
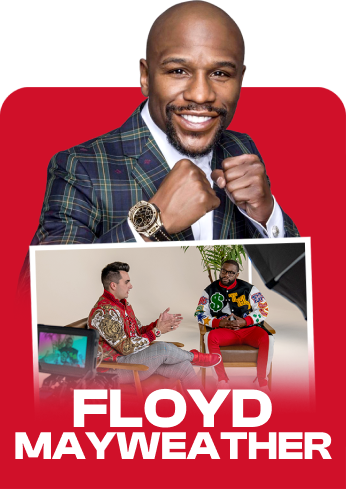
His A-list clients and partners such as Hollywood Actors, Athletes such as Floyd Mayweather, Olympians, NFL Super Bowl Champions and famous industry experts such as Les Brown. He’s helped over 40,000 companies grow, he’s often interviewed in magazines such as Forbes, Inc, Entrepreneur and currently runs a 100 employee company that was awarded the Inc 5000 last year.
His board members and partners including famous entrepreneurs such as Kevin Harrington from Shark Tank.
Rudy’s grown revenue to 1 Million $ per day, and spent over $200,000 per day profitably on Facebook ads! If you want to learn viral marketing, brand domination & the latest trends with influencer marketing, social media and content creation, look no further and get ready to discover the Red Life with Rudy Mawer!
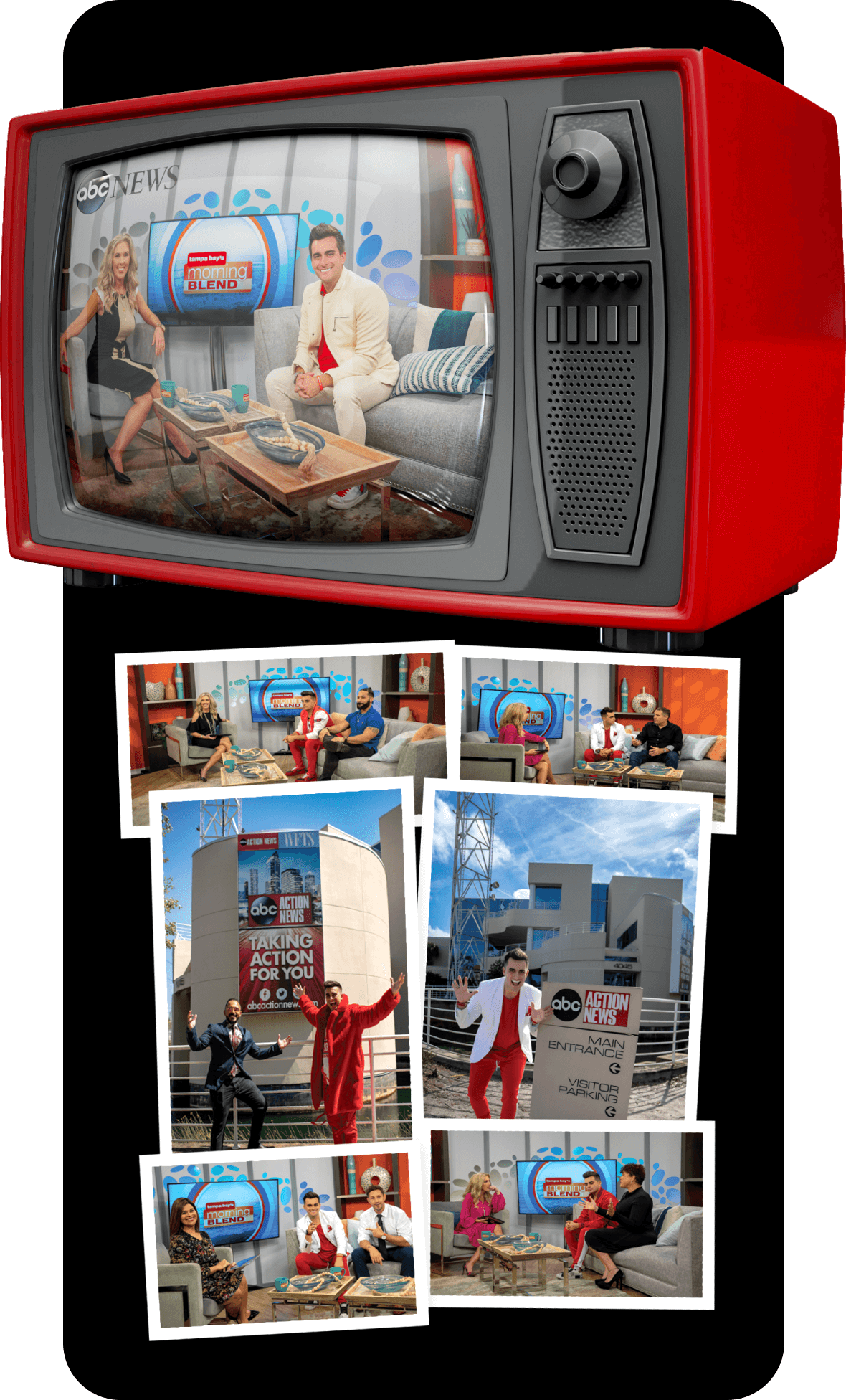
Rudy has spoken live on numerous channels, including CBS, NBC, ABC, & Good Morning LALALAND…
A morning blend to talk about business, social media, marketing, wealth, and everything in between.
Best part is Rudy brings on clients to discuss their business.

Sign up and get daily tips on ads, funnels and marketing strategies to scale your business…
Fill in your details and we’ll get back to you in no time.